Introduction to Urgent Care Billing
Urgent care billing plays a major role in the financial performance of urgent care centers. Clinics handle high patient volume, quick treatments, walk-in visits, and insurance verification on the spot. A streamlined urgent care billing process supports smooth reimbursement, accurate claim submission, and efficient collection of payments. Clinics require strong workflows for coding, documentation, charge capture, and claim follow-through to maintain revenue performance.
Importance of Urgent Care Billing Services
Urgent care billing services help clinics reduce administrative mistakes, improve coding accuracy, optimize payer communication, and support compliant claim submission. High-quality billing services improve denial management, enhance cash flow, strengthen claim success rate, and support long-term financial stability. Clinics depend on urgent care billing services to handle complex payer rules, coverage verification, procedure coding, and payment posting. A professional billing team ensures improved performance for every urgent care visit.
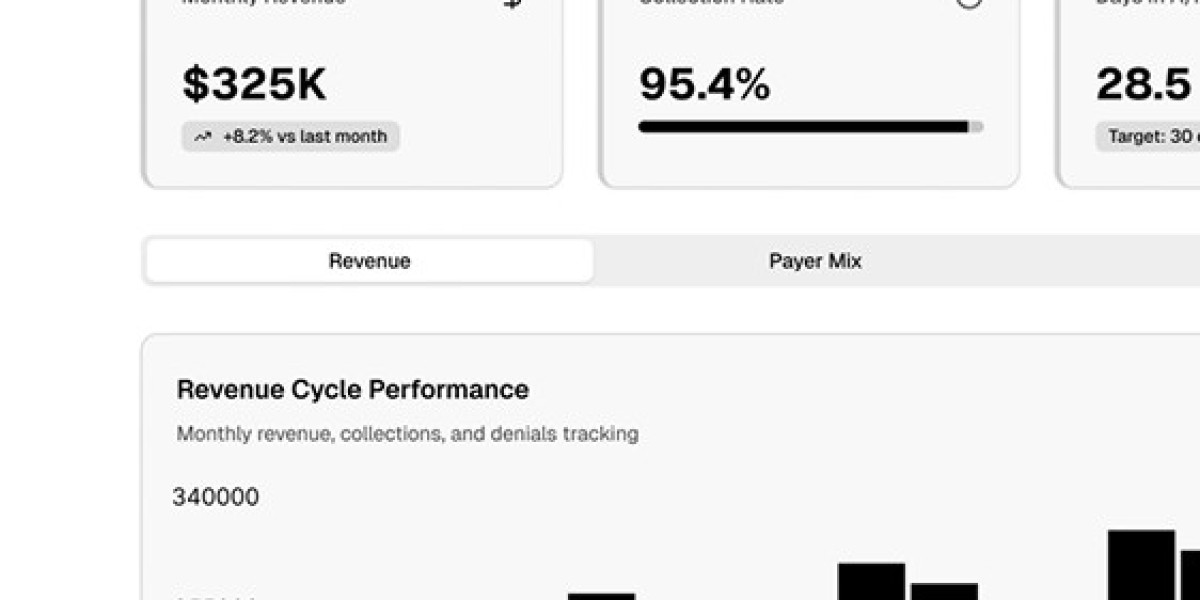
Role of Urgent Care RCM
Urgent Care RCM (Revenue Cycle Management) covers every step from patient registration to final payment collection. RCM services support scheduling, eligibility checks, coding review, charge entry, claim submission, denial tracking, AR follow-up, and payment posting. Urgent Care RCM ensures complete financial visibility and stronger reimbursement outcomes. Clinics using specialized RCM systems experience fewer revenue leaks, improved coding accuracy, faster claim processing, and better control over operational workflows.
Urgent Care Billing Challenges
Clinics face difficulties due to high patient turnover, limited documentation, rapid diagnosis cycles, and diverse procedure types. Missing coverage details, incomplete codes, incorrect urgent care CPT coding, and payer-specific requirements delay payments. Urgent care billing services solve these issues through detailed verification, accurate charge capture, error identification, and clean claim submission.
Understanding Urgent Care CPT Coding
Urgent care CPT coding identifies specific treatments, procedures, and services offered during each visit. Accurate CPT selection supports proper reimbursement. Common urgent care CPT coding categories include evaluation codes, diagnostic tests, therapeutic procedures, injections, laceration repairs, fracture treatments, and wound care services. Correct modifier usage supports accurate claim adjudication. Errors in urgent care CPT coding reduce payment accuracy and increase denials.
Urgent Care EHR Integration for Billing
Urgent care EHR systems help clinicians document services, review patient history, and capture treatments. Integrated EHR improves coding accuracy, supports automated charge entry, enhances eligibility verification, and provides real-time documentation support. Urgent care EHR helps billing teams access complete notes, lab results, imaging details, provider signatures, and encounter summaries. Efficient EHR workflows reduce documentation gaps and support error-free claims.
Urgent Care Revenue Cycle Management for Faster Payments
Urgent Care Revenue Cycle Management improves payment speed, enhances coding quality, and supports compliance. RCM teams monitor each claim from initial submission to final settlement. Revenue Cycle Management offers detailed analytics, supports performance reporting, identifies denial trends, improves documentation quality, and supports strong payer negotiation. A structured RCM model reduces revenue loss for clinics.
Benefits of Outsourcing Urgent Care Billing Services
Outsourcing urgent care billing services helps clinics focus on patient care. Expert billing teams handle coding reviews, chart audits, claim scrubbing, payer communication, denial appeals, and AR follow-ups. Outsourcing benefits include higher accuracy, improved collection rate, consistent compliance, faster turnaround time, reduced administrative pressure, and cost-efficient operations. Clinics using outsourced urgent care billing services gain better financial predictability.
Urgent Care Billing Workflow Overview
A strong workflow improves urgent care performance:
Patient check-in
Eligibility confirmation
Provider documentation
Urgent care CPT coding
Charge entry
Claim creation
Submission to payer
Denial review
Resubmission or appeal
Final payment posting
Each step requires accuracy to avoid claim delays. Urgent care billing services support every stage through auditing, validation, error correction, and reporting.
Urgent Care RCM Technology Tools
Technology supports billing efficiency. Tools include EHR systems, claim scrubbing tools, charge capture apps, denial dashboards, AR automation tools, and payment portals. These tools support accurate urgent care billing, improve cash flow, reduce manual workload, and enhance documentation quality.
Impact of Clean Claims on Urgent Care Billing
Clean claims reduce payment delays. Urgent care billing services ensure correct patient details, accurate urgent care CPT coding, complete documentation, proper modifiers, correct payer rules, and timely submission. Clean claims improve payer acceptance rates and support faster reimbursements.
Urgent Care Revenue Cycle Management Compliance Requirements
RCM programs follow rules set by CMS, private payers, HIPAA, and coding guidelines. Compliance protects clinics from audits. Correct coding, precise documentation, proper signatures, and accurate charge capture support compliant claims. Urgent care billing services help clinics stay audit-ready.
Improving Documentation Quality for Urgent Care RCM
Provider documentation supports coding accuracy. Detailed notes describing symptoms, diagnosis, treatment, and follow-up improve coding reliability. Documentation quality influences reimbursement success. Urgent care EHR tools support documentation completeness, generate templates, and reduce errors.
Conclusion
Urgent care billing supports efficient clinic operations. Accurate urgent care CPT coding, strong RCM processes, reliable EHR documentation, and specialized billing services improve reimbursement results. Clinics using urgent care billing services experience better claim acceptance, improved cash flow, stronger compliance, and long-term revenue stability. A structured Urgent Care Revenue Cycle Management approach enhances financial performance for every patient encounter.